Abstract

Introduction: With a high risk of morbidity and mortality, gastrointestinal bleeding (GIB) is a common cause of hospitalization, with transfusion considered the standard of care. Urgent treatment of a GIB can be challenging for many patients, such as Jehovah's Witnesses, who cannot accept transfusion of red blood cells due to religious convictions. We developed a clinical pathway to manage GIB in patients in whom transfusion is not an option, with hematologists providing a crucial role in managing anemia, coagulopathies, and reversal agents.
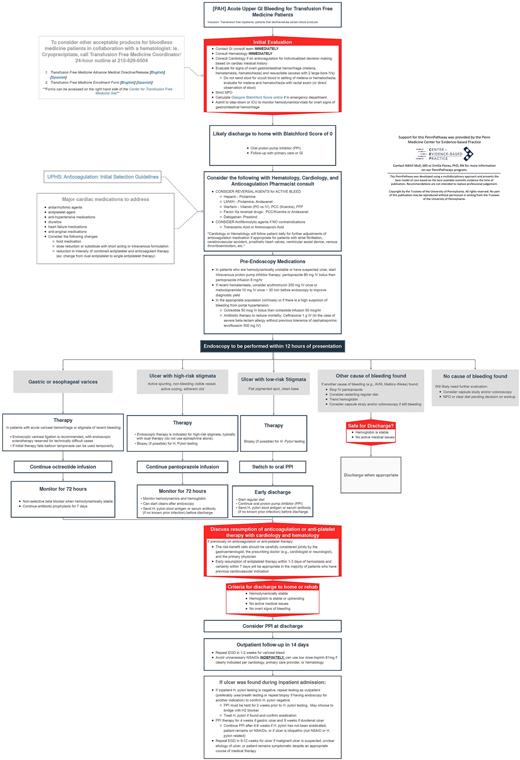
Our Transfusion Free Medicine (TFM) Program at Pennsylvania Hospital sees 1200 Jehovah's Witness patients annually. We were asked to develop a clinical pathway to share throughout the University of Pennsylvania health system due to our 100% survival rate with GIB in Jehovah's Witnesses spanning two decades. The pathway we created incorporates basic patient blood management strategies focusing on rapid interventions to control ongoing blood loss, correcting coagulopathies, and the utilization of pharmacologic agents to enhance hemostasis.
Methods: A multidisciplinary team of specialists, including physicians, advanced practice providers from hematology, gastroenterology, cardiology, interventional radiology, and members of the TFM program, was convened. Practicing Jehovah's Witness coordinators were specifically included to educate and counsel patients and providers on medical practices acceptable to Jehovah's Witness.
A literature review was performed to collate evidence-based practices for managing GIB. The review informed the development of the clinical pathway. Dissemination and access to the pathway included uploading a schematic onto a shared health system clinical care platform (Dorsata). The tool provides clinical decision support to providers by standardizing the approach to triage, navigation, and multi-modality treatment. The pathway structure is based on either upper or lower gastrointestinal bleeding. Implementation included clinical decision support built within the electronic medical records platform (EPIC) using smart phrases. These interventions facilitated gastroenterology, hematology, interventional radiology cardiology, and transfusion-free medicine referrals.
Results: The developed clinical pathway for upper GIB is depicted below with plans to track patient outcomes as it is used more frequently throughout the health system.
Conclusion: We developed and piloted a clinical care pathway to manage GI bleeding in patients who can not be transfused by leveraging expertise from a multidisciplinary team. Differences from the standard GI pathway where transfusion support is recommended include the essential role of the hematologist, cardiologist, interventional radiologist, and gastroenterologist to advise alternatives. The Cardiologist's role was essential to assist with reversal agents and determine the modification or withholding of cardiac medications when profound anemia occurs. These simple patient blood management strategies in the pathway have been successful, so much so that we believe they can be utilized in all patients with GIB. This pathway may also eliminate or reduce the need for unnecessary transfusion support, improve patient outcomes and create a more collaborative approach to treating gastrointestinal bleeding when transfusion is not an option.
Disclosures
No relevant conflicts of interest to declare.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal